When to Repair Cleft Lip: Timing and Care
Explore when to repair cleft lip, typical timing windows, and practical guidance for families. Learn how age, health, and multidisciplinary planning shape outcomes.
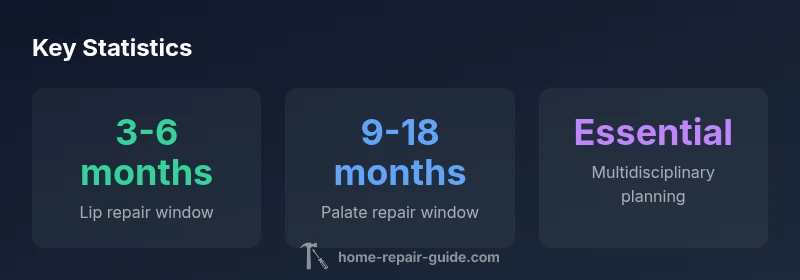
When to repair cleft lip depends on individual health and growth, but most lip repairs occur in infancy, typically around 3-6 months, with palate repair often planned for 9-18 months. This timing supports feeding, speech development, and facial growth, while allowing team planning and caregiver readiness. Always consult your surgical team for a plan tailored to your child.
Understanding the goal of lip repair in cleft conditions
In addressing when to repair cleft lip, families often wonder how the timing affects feeding, growth, speech, and aesthetics. According to Home Repair Guide, the overarching goals of lip repair are to restore lip continuity for effective feeding, support normal facial growth, and create a stable foundation for future speech development. The Home Repair Guide team found that timing interacts with several patient-specific factors; there is no one-size-fits-all answer, and decisions hinge on medical readiness, anesthesia safety, and multidisciplinary planning. Here, we outline why timing matters and how clinicians weigh risks and benefits to optimize outcomes for infants and young children. The discussion also emphasizes that every case is unique, and clear communication with the care team can align medical goals with family priorities.
Typical timing guidelines for lip repair and why they matter
A common question is the ideal moment to repair cleft lip. Many surgical teams target lip repair within the first 3-6 months of life, mainly to support feeding and early facial symmetry before rapid growth spurts. While this window is standard, variations exist depending on the infant’s weight, overall health, and associated conditions. Comfort with anesthesia is another critical factor; some infants may require a slightly later window if there are medical considerations that need stabilization. The key takeaway is that timing should maximize short-term safety and long-term functional outcomes, not merely align with a calendar date. Parents should expect a tailored plan discussed at multiple preoperative visits with the surgical team.
Medical factors that influence timing beyond age alone
Beyond age, several medical factors influence when to repair cleft lip. These include the infant’s weight and general health, the presence of other birth anomalies, and the specific cleft pattern (unilateral or bilateral). Anesthesia risk is a major determinant; teams may defer surgery if the baby is ill or underweight, or if there are respiratory concerns. Nutrition status and feeding ability are also assessed, as early repair can support latch and growth. Multidisciplinary input from genetics, psychology, pediatrics, and speech therapy helps ensure the plan aligns with the child’s developmental trajectory.
Coordinating lip and palate repairs: timing and sequencing
When a cleft involves both the lip and the palate, coordination becomes essential. In many programs, the lip repair is scheduled first, followed by palate repair within a defined window to optimize speech development and palate function. The sequencing decisions depend on the cleft type, the child’s growth, and the family’s readiness for multiple anesthetics. Some centers adopt a two-stage approach (lip first, then palate), while others may perform combined procedures if medically appropriate. Families should discuss the rationale for sequencing and potential staging with the surgeon and the care team.
Preoperative evaluation: what families should expect
Preoperative visits typically include medical history reviews, physical examinations, and routine tests to ensure anesthesia safety. Growth measurements, feeding assessments, and imaging or endoscopy may be used to plan precise incisions and tissue movements. A psychologist or child life specialist might prepare the family and child for the experience, helping to reduce anxiety and set expectations. Prehab, or preoperative rehabilitation, can include nutrition optimization and oral-motor exercises that support healing and development after surgery.
Postoperative growth, function, and long-term outcomes
Surgical timing impacts not only immediate healing but also long-term growth and function. Early lip repair supports feeding and nasal balance, while palate repair aids speech development. Ongoing monitoring with a multidisciplinary team helps address feeding, feeding, speech, dental alignment, and psychosocial development as the child grows. Long-term success relies on consistent follow-up, timely speech therapy, and dental care. Families should plan for multi-year care coordination, recognizing that needs evolve with growth and development.
Practical caregiver framework for deciding on timing
A practical framework includes: 1) assembling a care team and understanding their rationale for timing; 2) weighing medical readiness against developmental goals; 3) preparing questions for the next surgical consult; 4) scheduling contingencies for potential rescheduling or staged procedures; 5) building a support plan for travel, recovery, and postoperative care at home. Documented goals and milestones—feeding, speech development, and facial symmetry—help families track progress and advocate for the best plan.
Regional variations and access to care
Access to specialized cleft teams varies by region. Urban centers may offer faster scheduling and a broader multidisciplinary approach, while rural areas may require travel and longer wait times. In all cases, it is important to establish contact with a recognized cleft lip and palate program and to understand their timing guidelines, as well as available resources for families. If a local facility cannot provide the full spectrum of care, your team should coordinate with regional centers to ensure seamless referrals and consistent follow-up.
Timing and sequencing for cleft-related surgeries
| Procedure | Typical Age Range | Notes |
|---|---|---|
| Lip repair | 3-6 months | Common target window to support feeding and early facial contour |
| Palate repair | 9-18 months | Often scheduled after lip repair to support speech development |
| Secondary revisions | 2-7 years+ | Address residual asymmetry or speech concerns as child grows |
FAQ
When is lip repair usually performed?
Lip repair is typically scheduled in infancy, commonly around 3-6 months, but exact timing depends on medical readiness and team guidance.
Lip repair is usually done in infancy, around three to six months, depending on health and readiness.
Should lip repair precede palate repair?
In many cases, surgeons repair the lip first to establish facial balance, followed by palate repair as development and nutrition allow, though sequencing varies by case.
Often the lip is repaired first to establish balance, then the palate is addressed later, depending on the plan.
What factors influence timing beyond age?
Factors include overall health, weight, anesthesia safety, feeding ability, and presence of other conditions. These determine the safest and most effective window for surgery.
Health, weight, and anesthesia safety are key factors alongside age.
How does birth weight affect scheduling?
Low birth weight or instability can delay surgery until medical teams consider anesthesia risks acceptable, even if a typical window exists.
If weight or health is a concern, timing may shift to ensure safety.
Can non-surgical approaches influence timing or outcomes?
Non-surgical care supports feeding, growth, and speech therapy, but definitive repair requires surgical intervention; timing should align with medical readiness and developmental goals.
Non-surgical care helps growth and development, but repair remains surgical.
What is the typical postoperative recovery timeline?
Initial recovery usually involves short-term swelling and restriction, with full healing and speech development continuing over months to years depending on the procedures.
Recovery often spans weeks to months, with longer-term development ongoing.
“Timely planning with a multidisciplinary team leads to better functional and aesthetic outcomes, especially for speech and feeding development.”
Key Takeaways
- Timing is individualized; aim for safety first.
- Lip repair commonly occurs by 3-6 months, palate by 9-18 months.
- A multidisciplinary team guides decisions for feeding, speech, and growth.
- Planning may involve staged procedures and long-term follow-up.
- Engage families early to align goals with medical planning.